

Semaglutide (GLP-1) and glucagon-like peptide 1 are short, natural peptides. The naturally occurring hormone is only 31 amino acids in length, with a primary physiological function to lower blood sugar levels by naturally increasing insulin secretion. It also appears to protect beta-cell insulin stores by promoting the transcription of insulin genes and is associated with neurotrophic effects in the central nervous system and the brain. Studies in the GI system have observed that Semaglutide may significantly reduce appetite by slowing gastric emptying and bowel motility. Preliminary studies have also suggested the potential effects of Semaglutide on the heart, fat, muscles, bones, liver, lungs, lungs, and kidneys.
SYNONYMS: GLP-1, proglucagon (72-108), glucagon-like peptide-1
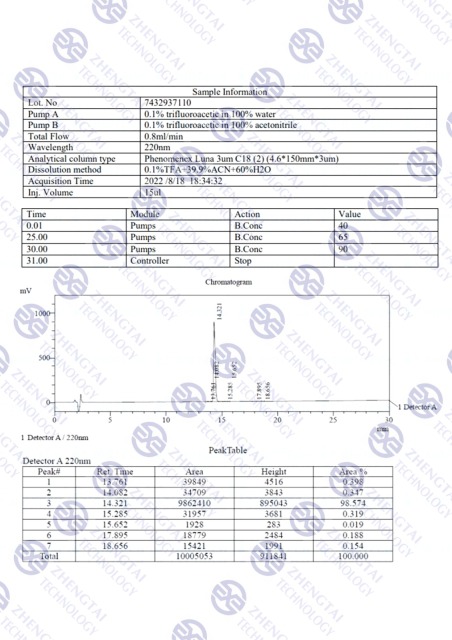
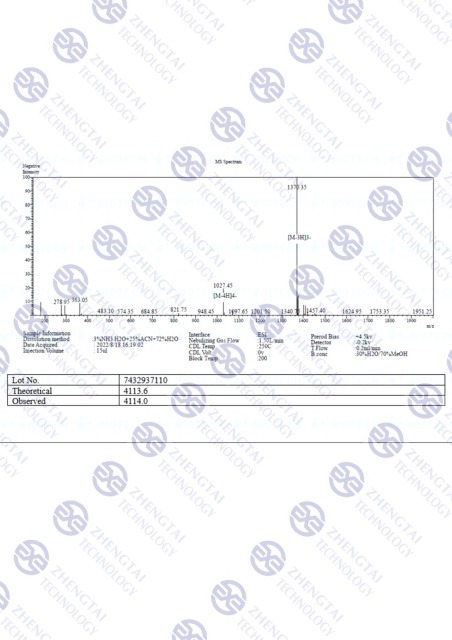
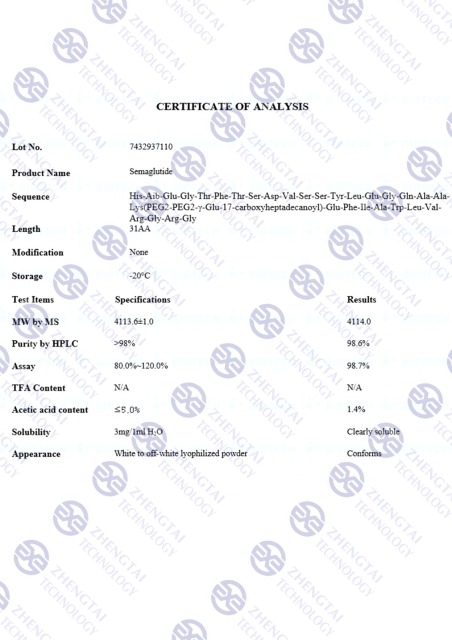
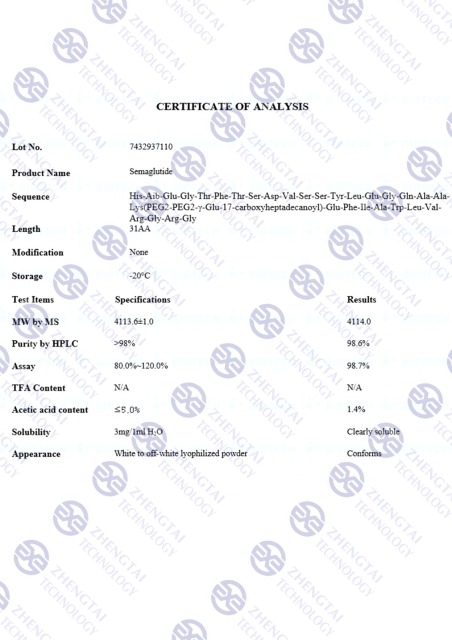
MOLECULAR FORMULA: C187H291N45O59
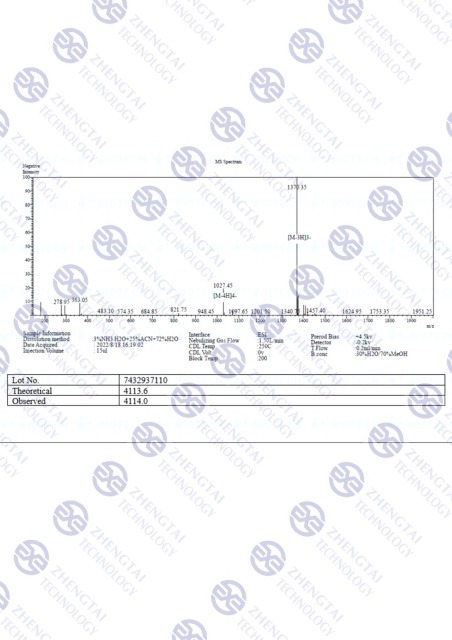
MOLECULAR WEIGHT: 4113.64 g/mol
SEQUENCE: HXEGTFTSDV SSYLEGQAAK EFIAWLVRGR G
PUBCHEM: CID 56843331
CAS NUMBER: 910463-68-2
RECONSTITUTION: Required
SEMAGLUTIDE AND THE INCRETIN EFFECT
According to Holst, the most widespread association with Semaglutide is the “incretin effect.”[1] Incretins are a group of metabolic hormones released from the gastrointestinal tract that lower blood sugar (sugar) levels. Semaglutide appears to be one of the two most common and essential hormones that stimulate incretin action in the rodent model (the other is GIP). GIP circulates at about 10 times the concentration of Semaglutide, but there is evidence that GLP-1 may be more potent than GIP, especially when blood glucose levels are relatively high.[2] The researcher also notes that “Decreased secretion of GLP-1 may contribute to the development of obesity, and exaggerated secretion may be responsible for postprandial reactive hypoglycemia.” Semaglutide receptors have been identified on the surface of pancreatic beta cells, suggesting that Semaglutide may directly stimulate insulin exocytosis from the pancreas. In combination with the sulfonylurea substance, Semaglutide has been suggested to increase insulin secretion. Various potential nutritional effects include a possible increase in protein synthesis, decreased proteolysis, and increase in amino acid uptake by skeletal muscle. It is hypothesized that the peptide interacts with the GLP-1 receptors in the pancreas, potentially stimulating insulin production in pancreatic beta cells and possibly suppressing glucagon production by pancreatic alpha cells. According to the research teams exploring this potential, the impact of Semaglutide appears to act in a glucose-dependent manner. Furthermore, it is suggested that the peptide potentially aids in reducing the postprandial glucose spike, which hypothetically happens immediately after a meal. Studies have posited that it appears to slow gastric emptying, potentially by up to 38%, within the initial hours following a meal.
SEMAGLUTIDE AND BETA CELL PROTECTION
Studies in animal models suggest that Semaglutide may stimulate the growth and proliferation of pancreatic beta cells and the differentiation of new forms of beta cells, precursors of pancreatic duct epithelium. Studies further theorize that Semaglutide may inhibit beta-cell apoptosis. These effects have the potential to upset the average balance between beta-cell growth and death. In terms of development, these research results posit the peptide’s potential to treat diabetes and protect the pancreas from attacks that damage beta cells. One particularly compelling study has indicated that Semaglutide appears to inhibit beta-cell death caused by elevated levels of inflammatory cytokines. In fact, in type 1 mouse models with diabetes, it was observed that Semaglutide appeared to protects islet cells from destruction, and therefore it may be a valuable tool in practice to prevent the onset of type 1 diabetes.[3] The scientists suggested that “It is possible that such combined therapy could become a new strategy to defeat T1DM in humans.”
SEMAGLUTIDE AND APPETITE
A study of mouse models suggests that administration of Semaglutide in the brain of mice may reduce the driving device and may inhibit food intake.[4] Semaglutide seems to induce satiation, reducing hunger instincts. Recent clinical trials are shown in the mouse where two-day management of the GLP-1 receptor agonist may cause gradual weight loss. This weight loss may lead to a significant improvement in cardiovascular risk factors and a decrease in hemoglobin A1C levels for a long time.
Evidence from studies implies a potential link between the activation of GLP-1 receptors in the central nervous system, specifically in reward-related brain areas, and the modulation of appetite through GLP-1 receptor agonists.[5] In more specific terms, it is hypothesized that GLP-1 receptor agonists may interact with neurons located in the arcuate nucleus of the hypothalamus. These particular neurons appear to play a role in regulating appetite and hunger and are posited to express proopiomelanocortin and cocaine- and amphetamine-regulated transcript (POMC/CART). It is suggested that the potential activation of POMC/CART neurons by Semaglutide, a GLP-1 receptor agonist, may induce satiety while indirectly inhibiting the release of neuropeptide Y (NPY) and agouti-related peptide (AgRP), which appear to be peptides that may promote hunger. Furthermore, studies propose that GLP-1 receptor agonists, such as Semaglutide, may assist in mitigating the decrease in free leptin and potentially elevate levels of peptide YY (PYY) 3-36 during weight reduction.[6] In a specific study, it has been suggested that Semaglutide appears to mediate a potential 35% reduction in mean energy intake during ad libitum eating, as compared to placebo (1736kJ vs. 2676kJ).[7]
POTENTIAL CARDIOVASCULAR BENEFITS OF SEMAGLUTIDE
Currently, Semaglutide receptors are distributed throughout the heart, and appear to improve cardiac function in certain situations by increasing heart rate and lowering left ventricular end-diastolic pressure.[8] A rise in end-diastolic pressure is often associated with left ventricular hypertrophy, cardiac remodeling, and ultimate heart failure. Recent studies suggest that Semaglutide may reduce the overall damage caused by a heart attack. The peptide appears to improve glucose uptake into the heart muscle; this helps the struggling ischemic myocardium maintain function and obtain the nutrients needed to avoid programmed cell death. Increased glucose uptake in these cells appears to be independent of insulin. High doses of Semaglutide in dogs have exhibited apparent improved and reduced LV performance and systemic vascular resistance. The latter effect may help lower blood pressure and relieve stress. This process, in turn, may help reduce the long-term consequences such as LV remodeling, vascular thickening, and heart failure. According to Dr. Horst, administration of GLP-1 after heart injury consistently appeared to improve myocardial performance in both experimental animal models and patients.
SEMAGLUTIDE AND THE BRAIN
There is potential evidence that Semaglutide may help to enhance learning and protect neurons from neurodegenerative diseases such as Alzheimer’s. One study has posited that Semaglutide may enhance associative and spatial learning in mice and improve learning disabilities in mice with specific gene defects. In rats that overexpress Semaglutide receptors in particular brain areas, both learning and memory appear to be significantly better than normal controls.[9] Further research studies of mice indicated the peptide’s potential to protect from immunotoxic neurons. Interestingly, Semaglutide and its analog exendin-4 have been reported in mouse models to apparently reduce amyloid-beta levels in the brain. The beta-amyloid precursor protein found in neurons is the primary component of the plaques observed in neurodegenerative disease.[10]
It remains to be seen if preventing amyloid-beta accumulation can protect against the effects of Alzheimer’s disease. Still, this research is, at the very least, a tantalizing clue as to how scientists may intervene in the progression of mild cognitive impairment to whole Alzheimer’s disease. Semaglutide (GLP-1) has so far been reported to exhibit minimal to moderate side effects and low oral and excellent subcutaneous bioavailability in mice, according to laboratory studies.[11]
SEMAGLUTIDE AND CAMP SIGNALING AT THE GLP-1 RECEPTORS
As noted earlier, GLP-1 receptors are G-protein-coupled receptors (GPCRs) that are considered to be located on the surface of various cells, including pancreatic beta cells, brain neurons, and cells in the gastrointestinal tract. When Semaglutide potentially binds to GLP-1 receptors, it may trigger a cascade of intracellular events. It is hypothesized that semaglutide possibly binds to the receptor’s extracellular domain, potentially leading to a conformational change in the receptor structure. This conformational change may hypothetically allow the receptor to couple with and possibly activate G-proteins inside the cell. It appears that Semaglutide may possibly facilitate the binding of the G-protein to the intracellular domain of the receptor, which may potentially lead to the exchange of GDP (guanosine diphosphate) for GTP (guanosine triphosphate) on the G-protein.[12]
The activation of the G-protein may subsequently trigger a signaling pathway involving the enzyme adenylyl cyclase. It is possible that the G-protein potentially activates adenylyl cyclase, resulting in the conversion of ATP (adenosine triphosphate) to cyclic AMP (cAMP). Increased cAMP levels then may also lead to the activation of protein kinase A (PKA). PKA, in turn, may phosphorylate various intracellular proteins, including transcription factors and ion channels. This hypothetical phosphorylation cascade may potentially result in numerous downstream effects, which we already mentioned.
Additionally, researchers have posited that Semaglutide may also exert potential by activating the GLP-1 receptor-mediated phosphoinositide 3-kinase (PI3K) pathway. This pathway may involve the activation of PI3K by the G-protein, potentially leading to the production of phosphatidylinositol 3,4,5-trisphosphate (PIP3). PIP3 may then activate downstream signaling molecules, such as protein kinase B (Akt). Hypothetically, Akt regulates various cellular processes, including glucose uptake, glycogen synthesis, and cell survival.[13]
SEMAGLUTIDE AND BETA-ARRESTIN SIGNALING AT GLP-1 RECEPTORS
Studies suggest Semaglutide may also potentially recruit beta-arrestins at the GLP-1 receptor, and it is hypothesized that beta-arrestins play a potential role in regulating GPCR signaling and internalization. If Semaglutide binds to the GLP-1 receptor, it may promote the recruitment and binding of beta-arrestins to the receptor. This recruitment may potentially lead to the desensitization and internalization of the receptor. Desensitization refers to the dampening of the receptor’s responsiveness to continuous stimulation, and it may occur through a process called receptor phosphorylation, where beta-arrestins might facilitate the addition of phosphate groups to specific sites on the receptor.
Researchers posit that following desensitization, the internalization of the GLP-1 receptor may occur. This process potentially involves the sequestration of the receptor into clathrin-coated pits, which then may form clathrin-coated vesicles. The internalized vesicles may transport the receptor to intracellular compartments for degradation or recycling back to the cell surface. The recruitment of beta-arrestins and the subsequent internalization of the GLP-1 receptor may contribute to the termination of signaling and enable the receptor to be available for future activation.[14]
It is worth noting that the recruitment of beta-arrestins at the GLP-1 receptor may also potentially initiate alternative signaling pathways independent of G-proteins. These beta-arrestin-mediated signaling pathways may elicit distinct cellular responses, including mitogen-activated protein kinase (MAPK) activation, which hypothetically regulates cell growth, differentiation, and survival.



